By Laura Gould, CCLS, MS
Understanding Precocious Puberty
Precocious puberty is early onset of hormones and sexual characteristics in girls before the age of 8 and in boys before the age of 9. It is important to note that children of some ethnic backgrounds may go through puberty sooner and a medical diagnosis should be made (Mayo Clinic, 2025)
Most children with this disorder have bone growth older than their chronological age and go through a growth spurt early which may result in initially being taller than peers at a young age. However, individuals with precocious puberty often stop growing before reaching their full genetic height potential. There are many potential causes of precocious puberty which an endocrinologist may investigate by doing lab work, a bone age x-ray of the hand, and/or an MRI of the pituitary gland. Causes may include tumors or growths of the ovaries, adrenal glands, pituitary gland, or brain, or central nervous system abnormalities, family history, or certain rare genetic syndromes. However, in most cases, no cause can be found for the disorder (CHOP, 2025).
Emotional and Developmental Impact
Advanced bone age can impact a child physically as well as psychologically. Growing faster than peers can make children taller initially and stand out from peers but then they stop growing sooner and may be shorter than peers later. In addition to an early growth spurt, children with precocious puberty may start developing breast buds, pubic and body hair, and body odor. Sometimes young girls have started menstruating and need support for managing this in early elementary school. Due to “mature” physical appearance adults may perceive children with precocious puberty as older and expect the child to be meeting cognitive and emotional developmental stages that the child is not yet. Experiencing these hormones early can impact not only physical development but also emotional development. Experiencing hormones can be a difficult time for pre-teens and adolescents and may be even more difficult for young children with mood swings and increased agitation. Caregivers initially may not know what is happening with their child. Even after a diagnosis, children may have a hard time understanding what is happening to their bodies as they are growing sooner than caregivers, doctors, and children may have expected. Children with precocious puberty may become self-conscious of these changes.
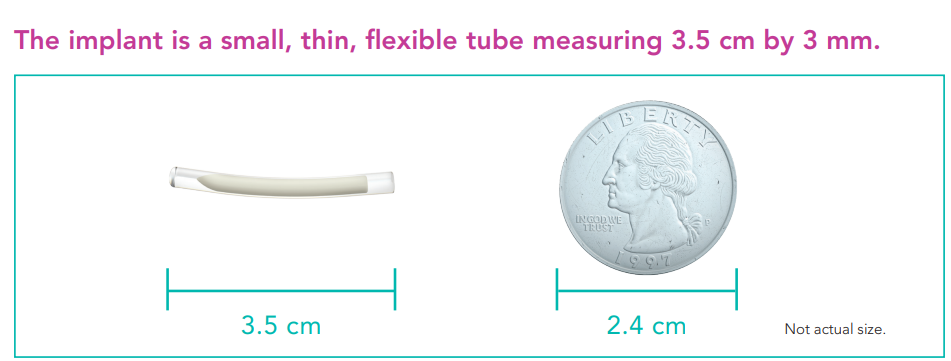
The Role of a Supprelin (Histerlin) Implant
One of the treatment options is a subcutaneous implant in the upper arm slightly above the elbow. It slowly releases a small dose of a drug that increases the body’s production of some hormones while decreasing others. The implant is replaced about every year and when the child has reached an age where they no longer need it, they will have it removed and go through puberty as is typical. Hormones are routinely monitored through blood work on patients to assess if the implant is working, needs to be replaced, or can be removed. Treatment is typically stopped around 11 years old for females and 12 years for males.
The Role of Child Life
Families look to child life for developmentally appropriate education and support. At times child life specialists educate the patient directly and other times provide the tools for caregivers to educate their child. The same is true when discussing puberty with children. This is amplified when it involves precocious puberty because children are younger, and families may not have prepared to have these conversations when body changes have started becoming noticeable to the child or others around them. When children come with some level of understanding about the appointment, then child life focuses on the steps of implant insertion procedure and developing a coping plan.
In the clinic where I work, child life specialists receive referrals to assist patients with preparation and procedural support when they are getting a Supprelin implant. A general surgeon places the implant which can be done in a clinic (without sedation) or on a sedation unit with mild, moderate, or deep sedation or in an operating room. The level of sedation depends on the anxiety of the patient, coping plan, and if the child is a candidate for sedation. Child life can often be involved in assessing the patients’ coping to see if the patient would benefit from a local anesthetic such as a numbing cream or lidocaine injection or if the patient will need more sedation to be able to cope with the procedure. Often caregivers and patients are surprised at how well they cope with numbing cream, lidocaine, and child life support during the procedure without needing more medication.
Many children and families are relieved to learn that other children are going through this same diagnosis.
Resources for Families
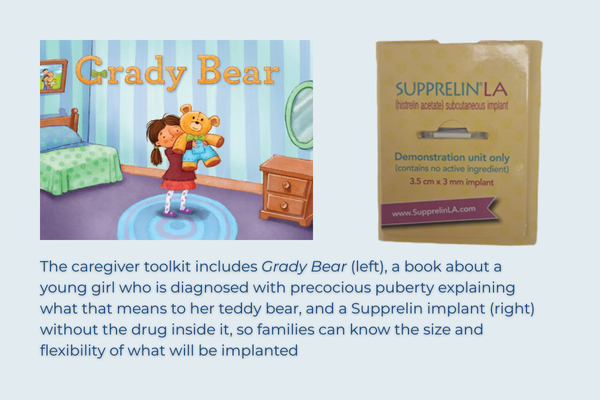
The generic implant is called a Histerlin implant, but the name brand Supprelin implant is commonly used. While I do not represent the company in any way, I appreciate the resources that the Supprelin company offers to caregivers and families prior to coming for an implant. Families can go on to the Supprelin drug company’s website to order free resources. Families can order a caregiver toolkit to learn more. The kits are available in English and Spanish. This includes a book, an implant without the drug inside, and a video.
Another resource to puberty and body development is an audiobook exclusive on audible written and narrated by health educator Justine Ang Fonte, How To Talk To Your Kids About Sex. While it has “sex” in the title, many of the topics discussed focus on body part identification and development. I appreciate how Fonte discusses how to scaffold these conversations with toddlers through adolescence.
This audiobook is not only helpful for caregivers but also for health care professionals, including child life specialists, navigating conversations with young patients. It is best for caregivers and providers to listen to without the child and then decide which portions are best to tailor education to each child’s developmental needs.
Learning about precocious puberty helps children with this condition understand more about their bodies and development. Having developmentally appropriate conversations with caregivers and health care providers, including child life specialists, helps children to feel supported and opens the doors to future conversations about body development.
References
CHOP. 2025. Precocious puberty (Early puberty). https://www.chop.edu/conditions-diseases/precocious-puberty-early-puberty
Endo. 2025. SupprelinLA. Parent and caregiver videos. https://www.supprelinla.com/hcp/caregiver-resources/
Mayo Clinic. 2025. Precocious Puberty. Precocious puberty - Symptoms and causes - Mayo Clinic
This column represents only the personal views of the author, and the Association of Child Life Professionals does not endorse or sponsor the products or services mentioned. In addition, the author verifies that they have no affiliation with the companies or organizations related to the products and services mentioned in this article. If readers would like further information, they may contact Laura Gould at gouldl1@chop.edu